Bringing Bella Back
A six-year-old's fight against anti-NMDA encephalitis

Just days before Christmas in 2023, a previously healthy, five-year-old Bella suffered a seizure that sent her to Morgan Stanley Children’s Hospital of New York (CHONY). A follow-up appointment for outpatient neurology was scheduled to investigate a possible epilepsy syndrome. However, a few days later, the typically chatty preschooler had stopped talking and wasn’t able to follow commands.
Upon returning to the hospital, Wendy Silver, MD, a pediatric neurologist at CHONY and consulting neurologist at Blythedale, performed a lumbar puncture on Bella at CHONY, and diagnosed her with anti-NMDA encephalitis, a serious condition that occurs when the immune system mistakenly targets neurons in the brain, causing inflammation.
“I remember doing the lumbar puncture on Friday and then immediately starting her treatment on Saturday.” For Silver, starting IVIG treatment immediately to reduce the inflammation in her brain, decrease her autoantibody levels, and restore her immune balance was crucial. Bella was deteriorating in front of her.
After two months of intensive critical care at CHONY, and once she was medically stable to be transferred, Bella was admitted to Blythedale for the next stage of her recovery.
"The NMDA receptors are crucial for learning, memory, and other cognitive functions," said Dr. Ying Chuu, attending physician at Blythedale Children’s Hospital. "Here at Blythedale she was able to get the intensive rehabilitation she needed to get her physically ready when she emerged (from her catatonic, non-responsive state)."
"When Bella came to Blythedale, she was dependent for all her cares,” said Susan Quinn, nurse practitioner at Blythedale. "Bella was not able to speak or communicate her wants or needs. She was not able to follow commands or walk. She required gastrostomy feeds, as she could not eat by mouth, and she had minimal interaction with her environment.”

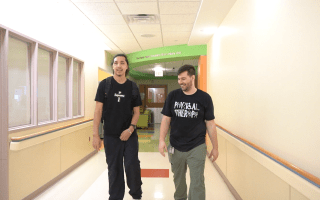
While at Blythedale, Bella continued to receive her monthly medical treatments at CHONY, including plasmapheresis, IVIG, steroids, and immune modulators. She would then return to Blythedale for her comprehensive rehabilitative therapies and medication management. She was followed closely not only by her clinical team at Blythedale, but also by her treatment team at CHONY, including Dr. Silver, and Dr. Oscar Gerdner, her psychiatrist. Both Dr. Gerdner and Dr. Silver provide in-house consulting services to the patients at Blythedale on a weekly basis. As they continued to follow Bella’s case, they saw that she wasn’t responding as they hoped to the medications.
"In this instance, the multidisciplinary care is really highlighted," said Dr. Silver, in reference to the vital collaboration of the psychiatrists at Columbia and Cornell with Dr. Gerdner at Blythedale. As Bella remained in a catatonic state, the physicians developed a plan to help her emerge.
“For catatonia, we try medication therapy first and, in Bella’s case, we tried really hard with high doses of medications to give her everything we could,” said Dr. Gerdner. “And at a certain point, after she had been stuck and frozen in this state, it occurred to us that when we reach that point with adults, we think about electroconvulsive therapy (ECT), which is a very tried and true treatment for catatonia that doesn't respond to medication treatment.”
ECT sends a brief electrical stimulus to the brain to reset it while the patient is under anesthesia, and is an approved treatment for those over the age of 12. However, there weren’t many studies on the response rate in younger children.
Bella’s family thought long and hard about the treatment.
“We prayed and ultimately said that this child needs to get her life back,” said Bella’s grandmother, Delores. In September 2024, Bella had her first ECT treatment.

Through a collaboration between the National Institute of Health, Children’s Hospital of New York, Weill Cornell Medical Center, and Blythedale Children’s Hospital, the teams met frequently to discuss how Bella was responding to treatments. In all, Bella received 22 electroconvulsive therapy treatments at Weill Cornell and returned to Blythedale for physical, occupational and speech therapies. Over the next five months, the team began to watch as Bella emerged from her catatonic state. Drs. Gerdner, Silver, and Chuu, and Nurse Practitioner Susan Quinn recall a very memorable telehealth call that all the treatment teams were on.
“It was Halloween, and Bella was in this pink dress, and grandma was blowing bubbles and Bella was popping them with her wand,” said Quinn.
Dr. Gerdner also remembers that meeting. “She started popping bubbles,” he said, noting the great emotion of the moment. “It was incredible to see it happen.”
Bella continued to make progress, working hard in her therapy sessions.
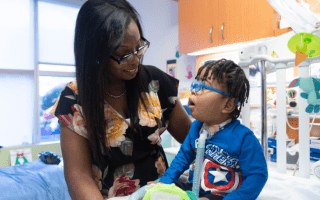
“I remember when I first saw her eating an Oreo cookie,” recalled Quinn. “She started walking, talking more each day, and participating in her daily activities, like showering and brushing her teeth. She was able to have her feeding tube removed. It was great to see her personality shine.”
In January, accompanied by her mom and grandma, Bella was discharged from Blythedale's inpatient program and transitioned to Blythedale’s Day Hospital program where she continues to receive therapies, and attends kindergarten at the Hospital's onsite Mount Pleasant Blythedale Union Free School District.
“That’s the thing about Blythedale," said Dr. Silver. "I've seen children come out of here looking much better than one would have thought when they came in. And I think Bella is definitely the epitome of that; to see her deteriorate and then come out the other end. And being here at Blythedale, I got to see that, and it's really just wonderful.”